Insurance Payers carry the brunt of the work to prepare for the No Surprises Act— but they aren’t in it alone. IT partners play a critical role in preparing medical claims processing workflows for NSA compliance.
Few situations are scarier than when a patient receives an unexpected medical bill in the mail. Oftentimes this is the result of surprise billing, which occurs when a patient unknowingly receives care from an out-of-network provider and is responsible for paying the balance.
Surprise billing can range from hundreds to thousands of dollars, leaving many Americans with nowhere to turn except for bankruptcy. A report in the American Journal of Public Health concluded that two-thirds of bankruptcies filed in America cite medical expenses as a cause.

In an effort to curb unexpected medical expenses, the U.S. Departments of Health and Human Services (HHS), Labor, and Treasury, and the Office of Personnel Management issued an update called the No Surprises Act (NSA). One of the main components of the NSA is to restrict the practice of surprise billing for both emergency and non-emergency situations.
This new rule aims to better protect Americans from medical-related financial hardship while placing the administrative and financial burden on insurance Payers.
So how are insurance Payers supposed to handle NSA updates?
How the No Surprises Act Affects Insurance Payers
Insurance Payers will take on the brunt of the work to process medical claims according to this new rule. This includes determining what is and is not considered a surprise bill, as well as what qualifies as emergency versus non-emergency services.
Medical claims processes are in need of simplification as they stand today. The NSA will add to the complexity and length of claims workflows, putting more strain on in-house talent. In addition to job stress, insurance companies will need to maintain a strong administrative workforce in an industry that’s expected to decline over time, according to the Bureau of Labor Statistics.
This leaves insurance Payers bending over backwards to accommodate the No Surprises Act.
Fortunately, insurance Payers don’t have to tackle it alone. IT partners such as Smart Data Solutions can work alongside insurance Payers to adapt their medical claims processing workflows to comply with the NSA—all while lowering administrative costs, improving accuracy, and speeding up turnaround time.
Working with an IT partner eases the burden of complying with the NSA by providing technical expertise to improve the necessary medical processing workflows.
4 Ways IT Partners Support Insurance Payers with NSA Compliance
- Improve workflows to incorporate NSA requirements.
IT partners who specialize in medical processing often embrace automation as a key component of success. Automating portions of workflows can support accurate and timely billing by determining the type of provider and location of services. Technology will be a key factor in adapting to the NSA requirements—and IT partners are a quick win for assessing workflows and improving them. Medical Economics summarized this,
“To provide the transparency and compliance the Act requires, Providers can look to readily available technology to ensure the right data is captured and routed to both patients and providers throughout the care journey.”
- Customize workflows to specific needs.
No matter what file format is required for your specific workflow, a true partner will be able to present data in any format you prefer. Our team at Smart Data Solutions is noticing that different entities appear to be pursuing their Qualified Payment Amounts (QPAs) in different ways. This is to be expected, which is why SDS is familiar with any format required. We can extract the correct data needed regardless of the type of file or structure.
- Determine Qualified Payment Amount (QPA).
Given that different vendors have their own unique approaches to determining QPAs, this is an area in which IT partners are especially helpful. Choosing to outsource QPA workflows lifts the burden of manual research off in-house teams. Your IT partner will be responsible for doing the research and incorporating data from nearby, ensuring the QPA is “Usual” and “Customary.” We can add the QPA and reason code to any claim, and move the QPAs from the Networks to the Payer, leaving your team with a final file in the exact format you need. Over time these workflows are improved with machine learning and automation to ensure accuracy and speed up the processing time.
- Proactively monitor changes and recommend improvements.
Perhaps the biggest benefit of tapping an IT partner to help navigate changes of the NSA is the proactive assistance in monitoring updates and ensuring compliance. Our sole responsibility is to enhance medical claims processing workflows, so our team always has an ear to the ground on updates that will impact processes. Our team of technologists determines if and how updates could affect our clients and prioritizes the next steps to remain compliant. Partnering with SDS means you’re always two steps ahead with a plan of action already prepared.
“The only constant in life changes,” Heraclitus famously said—and working in medical claims processing means you’re well-versed in navigating changes with rigor.
The No Surprises Act is yet another change we’ll all have to adapt to, but fortunately, we’re all in this together. Our team has planned for updates to help clients get ahead of these required changes.
We’re offering a free NSA consultation for insurance Payers to get ahead of the upcoming rule. Results of the consultation include:
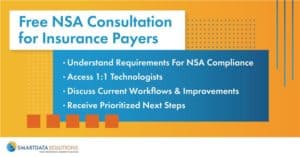
Time is almost up to prepare for NSA changes. Get started today by requesting a free consultation with Smart Data Solutions. Request a Consultation Here.
