Analyzing dental claims processing workflows for ways to optimize efficiency starts with a foundational understanding of the extensive journey a dental claim goes through before a patient receives the final bill.
Drafting the final dental bill requires the claim to go through 12 or so steps, providing many opportunities for error that ultimately can harm the turnaround time and efficiency of the process. With this in mind, Smart Data Solutions (SDS) crafted a workflow and proprietary software to curb the delay of dental claims processing and automate the journey of a patient’s final bill.
So what are the tools and methods a dental claims processor like SDS uses to create efficient dental claims processing? Let’s dive in.
How to Streamline the Dental Claims Processing Workflow
Several strategies help alleviate some of the gummed-up processes of claims management. Outsourcing, consolidation, and advancements in automation have all proven incredibly useful in streamlining the dental claims process for you and your company. Optimized processes help avoid common bottlenecks and errors that can delay the progress of dental insurance claims processing for your business.
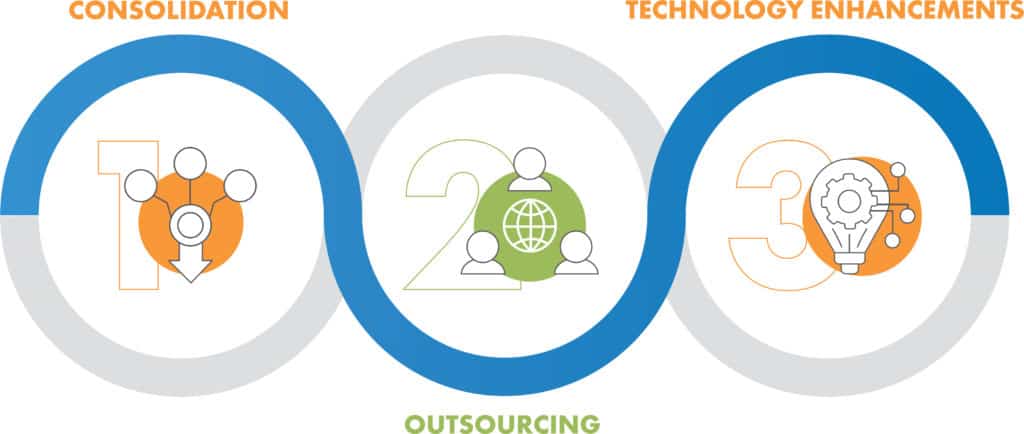
1. Consolidation
Processing dental claims can be extensive if there is not a fine-tuned workflow in place. In your dental claims processing workflow, monitoring and limiting the number of handoffs a claim goes through helps reduce the potential risk of human error.
While HIPAA does have regulations and rules set on how claims should be processed electronically, manual processes are always going to be part of the workflow to some extent. The more handoffs a claim passes through, the greater the chance of downstream errors. Consolidating handoffs is one of the benefits of outsourcing claims processing to an experienced vendor.
2. Outsourcing
When it comes to dental claims processing for your patients, hiring a business process outsourcing (BPO) vendor to take care of your claims management services can be greatly beneficial for efficiency and accuracy. From dental insurance correspondence to provider and member matching, to quality control, dental workflow automation and clearinghouse vendors can handle any step of the claims management process.
Partnering with a third party for claims management frees up time and space for in-house teams. This allows employees to focus on more strategic work than administrative processes. It also can offer financial savings by avoiding challenges such as turnover and training. On top of this, negotiation processes between payers and providers become easier with an outsourced team by your side that has historical industry connections and relationships. A representative looking out for both your providers and members creates efficiency and peace of mind.
3. Technology Enhancements
One of the most effective ways to improve efficiency and accuracy in the dental industry is automation. Advancements in optical character recognition (OCR) help streamline the data capture process in using different forms. Machine learning paired with AI helps ensure no data is missed, everything is accurate, and errors are caught before they get to the dental billing stage. Business-specific rules are used to match members and their providers by using a few data points like name and date of birth.
By utilizing machine learning, dental claim workflows can automate form variations by putting templates and automated processing in place. This allows the same process to be completed no matter what form is being scanned or input. AI avoids countless errors and misinformation by taking the proper fields from the form and matching them up into a standardized electronic format.
How Auto-Adjudication Can Improve Processing Dental Claims
Adjudicated claims can improve the general customer experience with faster, more accurate processing. To auto-adjudicate claims means to automate how the responsibility of the payer is determined. Upon reaching the payer, the claim will either be completely paid, denied, or the price will be negotiated based on the member’s health insurance coverage.
Payers, providers, and members will see an increase in faster, more accurately processed claims once auto-adjudication has been integrated within the claims processing workflow. When dental claims are processed faster, dental providers receive quicker payment, and insurance companies can have fewer pending claims outstanding, creating a win-win for all.
Smart Data Solutions and Automating Claims Processing
To many, the dental claims process is often overwhelming or inefficient, with errors and gaps frequently occurring. If you find yourself being challenged by the dental claims process, contact SDS for a consultation. Smart Data Solutions is a certified vendor of services ranging from automating how claim forms are read to processing members’ dental insurance with a claim. We help dental practices reach their fullest potential for patient care.
