As you begin planning for 2023, it is important to be aware of current trends in the market and what they could mean for your organization. Automation technology in healthcare continues to gain traction and popularity, making it a key component to begin implementing if you have not yet. Three of the hottest automation trends moving into the new year and beyond are Intelligent Automation, customizable technology, and customer insights.
-
Intelligent Automation:
Intelligent automation (IA) combines artificial intelligence (AI) elements such as natural language processing (NLP) and machine learning (ML) with automation. IA solutions orchestrate capabilities such as process mining, robotic process automation (RPA), optical character recognition (OCR), and business process management (BPM). IA applies algorithms to automate and continuously refine processes and entire workflows that may require judgment and can interpret both unstructured and structured data.
Intelligent automation can be implemented into multiple aspects of your healthcare workflow, whether it be in client care, administrative work, or claims processing. IA technology has continued to be a trend, with emerging technologies making previously tedious manual labor more efficient and cost-efficient.
Natural Language Processing (NLP) and Machine Learning (ML) are two IA technologies currently used throughout the healthcare industry. As defined by IBM, Natural Language Processing (NLP) gives “computers the ability to understand text and spoken words in much the same way human beings can.” When NLP is used from a data management perspective, it can learn to detect and categorize language patterns used in the industry, which helps isolate meaningful data. NLP technology can also be used for Payers taking the form of a virtual agent using conversational artificial intelligence to help connect Health Plan members with personalized answers at scale. The second technology being used is Machine Learning (ML). Machine learning can be used to process information and recognize patterns to analyze and categorize health care claims. The longer this type of IA is used, the more effective it becomes.
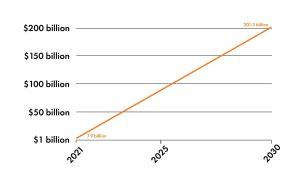
Intelligent automation is continually on the rise in healthcare, with projected growth in this area surmounting to millions of dollars in the coming years. An Acumen Research and Consulting study found that “artificial intelligence in [the] healthcare market size was valued at USD 7.9 billion in 2021 and will achieve USD 201.3 Billion by 2030 growing at 43.4 percent CAGR.” These markets continue to increase in value, and investment in these technologies can result in significant ROI for businesses. It is important to note that companies should consider the integration period before seeing their investment pay off. Deloitte advises to “factor in extra time for early adoption.” It states, “since the training of models is an ongoing process, expected return on investment (ROI) should include the time period and time frame.” As healthcare continues to move toward intelligent automation, it is a worthwhile investment that will save you money long term.
-
Customizable Technology:
As technology advances, customizable solutions become more accessible but also necessary to keep up with customer demands and trends. Technology that caters to the consumer has permeated every aspect of modern tech usage, leading to the need for customizable solutions, even within healthcare claims processing. According to Upptec, customers “are driving this digital shift with an ‘outside-in’ demand, where you may move away from a transaction focus to create holistic, compelling experiences.” So, what does that look like? Customers should be able to decide how they want to file claims and have the capability to report incidents digitally. This calls for cloud-based solutions and access to claim settlement tools, such as an app that can be easily accessed.
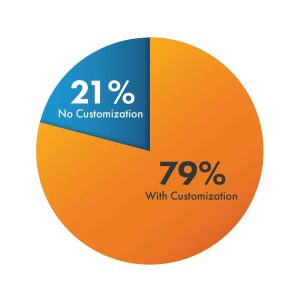
Introducing more customized solutions means that insurance Payers will have to optimize their processes, with a need for scalable technology and quicker processing times. As we move forward into the next year and beyond, keeping up with customizable technology is key to keeping up with the competition in the industry. According to Youbiquity Finance Report, “79 percent of consumers reported that their Providers offer some level of customization, while 21 percent indicated their Providers do not. If you are among the minority of Providers not personalizing your services, it is easy for customers to recognize the difference.”
Although personalized insurance products are relatively new, in the coming years, they will be “the new norm.” According to Upptec, customers will increasingly not only want automated and customized solutions, but they will expect them as the new industry standard. It was found in a recent Accenture report found that “80 percent of insurance customers want personalization from providers,” with this percentage very likely to increase in the coming years. Of this 80 percent, it was found that “…customers want you to share exclusive offers, recommendations, and services based on the individual’s needs and circumstances.” If you want to get ahead of the curve and increase customer satisfaction, now is an excellent time to start integrating more customizable technology.
-
Customer Insights:
Insurance claims provide valuable data that could be optimized to create profitability for both Payers and Providers while also benefitting customers. In an era where data is constantly accessible at the click of a button, it’s no surprise that customer data management and analysis are hot topics in the healthcare industry. Data management is critical for success, as it helps Providers anticipate consumer needs and act proactively to improve care, leading to better overall decision-making. Better decision-making leads to cost reduction, as it results in fewer visits to the doctor. If a medical issue can be properly diagnosed and handled within one visit to the office instead of two or more visits for the same issue, it saves time and money for the customer, Payer, and Provider. A study conducted by McKinsey found that “efficient big data analysis can save the U.S. medical industry $300 billion per year.” Tools to help manage customer data also create the opportunity to implement intelligent automation, another big industry trend described previously. IA technology can be beneficial when handling large volumes of data, as it can store, process, and analyze data more efficiently and effectively.
Safeguards are in place when collecting patient data, and consumers can trust that healthcare Providers keep their personal information safe, as HIPAA regulations require. It should always be communicated what kinds of data are being collected and analyzed and how this could potentially be shared when discussing with customers. KeyUA shares three ways to collect customer data safely and effectively: Customer Relationship Management (CRM) software, Electronic Health Records (EHR), or mobile apps. Commercial software is the most common in the current market, but customized tools are very beneficial and can improve the quality of services.
Intelligent automation, customizable technologies, and customer insights are essential to integrate into your business. When implemented, all three of these automation trends complement each other, as they help optimize business function and revenue growth while improving customer care.
To learn more about how Smart Data Solutions can help you to achieve your goals for 2023 with automated technology solutions, fill out our contact us form!
