Every institution is on the hunt for efficiency gains. Streamlining work and automating processes lowers costs and saves money. It’s no surprise that Healthcare Payers have made transformation and modernization a top priority in the years to come.
How does this play out in everyday work? There are many places an organization can modernize, but insurance Payers have focused on one key area: healthcare claims adjudication services. Companies typically don’t have the in-house technology to prepare claims for auto-adjudication on their own, such as using optical character recognition (OCR) to perform a detailed information check, which looks for diagnosis and procedure codes, and matches patient ID to their corresponding date of birth (DOB). The simplest solution to achieve modernization is to partner with a healthcare IT provider like Smart Data Solutions (SDS) to facilitate better collaboration among partners and prepare claims for auto-adjudication downstream.
Table of Contents
Automation: The Best Way to Enhance Claim Adjudication Services
Adding automation to claim adjudication benefits the front-end electronic data interchange (EDI) and the overall healthcare claim adjudication process. This results in more accurate information being fed into workflows and, ultimately, less manual effort spent verifying or correcting claims.
In this process, data validation runs both basic and detailed information checks on each claim, ensuring that there are no duplicate forms, DOB and Patient ID are successfully matched, and that personal information and plan IDs are accurate. Faster adjudication means faster routing. Intelligent automation can check more plans in a given period allowing for the entire routing and processing timeline to drastically speed up, ultimately saving time and resources.
4 Questions to Ask When Researching Claim Adjudication Services
Researching claim adjudication services can appear daunting, but keeping a few key points in mind will ease the intimidation. Consider asking these questions when evaluating potential partners:
-
Does this vendor specialize in healthcare and medical industries?
Plenty of automation services providers in the market will take on any client that walks through the door; however, it’s important to be confident in a partner’s ability to handle medical information — and all the nuances and regulations that go along with it. Ask for case studies that are comparable to your situation to evaluate whether this company has proven experience as a strategic partner in similar endeavors.
-
Does their team provide strategy and direction, implementation and execution, or all of the above?
When entering the claim adjudication automation space, you’ll need someone who’s able to assess your current situation, determine the most impactful next steps and influence the direction of the work based on what’s important to your business. Will these contractors give you strategy, direction, implementation, and more? Defining what they will be responsible for and what your company will handle can make a world of difference and can have a lasting impact on the effectiveness of your modernization.
-
How do they approach technology innovation in-house?
The healthcare claim adjudication process is rarely ready for an out-of-the-box solution or a “one-size-fits-all” approach. Your workflow may vary wildly from department to department, and you will need a company that can incrementally bolster your process. Ideally, they would have in-house innovation that can examine your systems, build on them, and continually work with your teams to ensure everything is running optimally. Systems can change based on new regulations or industry standards, so you want to employ contractors who can handle these developments and effectively insert them into existing systems.
-
Can they expand on their process for optimizing claim workflows?
As mentioned above, there is rarely an out-of-the-box solution for claim adjudication. If the team you work with can handle optimizing workflows, can they also expand on their process for doing so? A one-time fix likely won’t carry you through the next few years. As changes happen, will this partner be able to continue to work on the systems they have built, or will you be back to square one?
Questions like these will give you the insights necessary to feel confident about your partnership with whichever vendor you choose.
Intelligent Automation in Claim Adjudication Services Is Here To Stay
Efficiency is the hallmark benefit of intelligent automation. Claims specialists who embrace automation realize reduced workloads and internal friction; the C-suite sees increased savings and better patient satisfaction; and lastly, healthcare IT teams experience decreased friction in everyday work. There is no stopping the relentless advancements in automation because of the tangible benefits it brings.
Gartner’s 2022 Hype Cycle for U.S. Healthcare Payers stated:
“The combination of AI-driven decision-making and orchestration capabilities with automation technologies is an accelerator to optimizing and transforming processes throughout the enterprise.”
Gartner reported the current healthcare system is honing in on two areas: digital optimization and modernization and digital transformation and innovation. Healthcare IT leaders are continually challenged with increasing their reliance on automation to make claims processing more efficient. This focus has brought terms such as “hyper-automation” and “intelligent automation” to the forefront of the claims processing industry. This evolution of Healthcare IT will be increasingly reliant on trusted partners that have the technology and expertise required to integrate automated services into day-to-day businesses.
Partner with a Healthcare IT Provider to Advance Claim Adjudication Services
Healthcare Providers and insurance Payers can expedite their digital modernization by partnering with a healthcare IT provider, such as Smart Data Solutions, and see almost immediate ROI. SDS provides the technical prowess and the healthcare experience to empower healthcare, dental, medical, and pharmacy organizations through digital transformation.
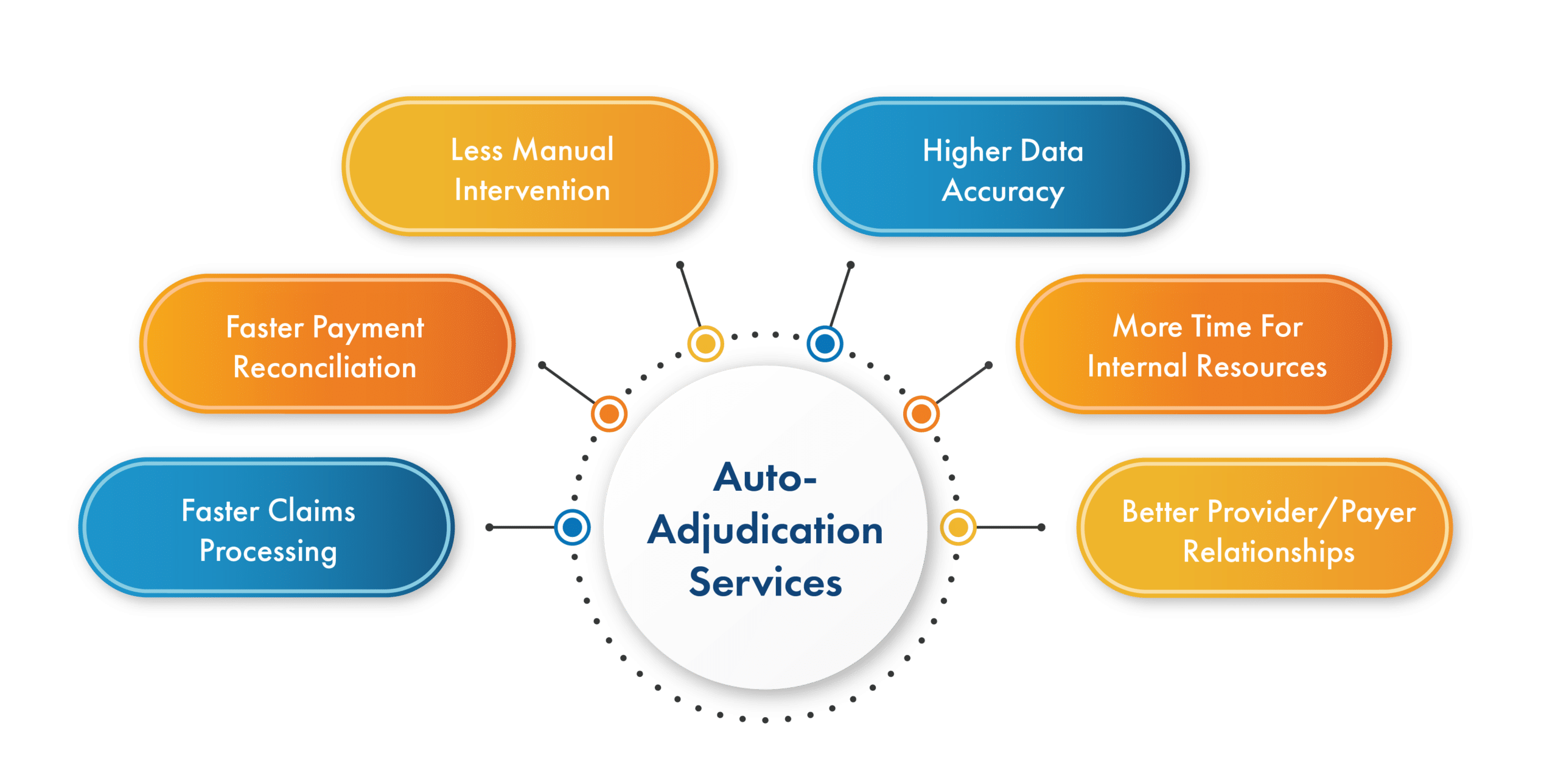
Our decades-long experience in the healthcare industry makes us the ideal companion for Payers and Healthcare Providers to leap into automated claim adjudication. The auto-adjudication services we provide benefit companies with:
- Faster claims processing
- Faster payment reconciliation
- Less manual intervention
- Higher data accuracy
- More time for internal resources
- Better Provider/Payer relationships
If you’re interested in securing a better workflow for claim adjudication, increased organizational efficiency, and better allocation of human capital, contact SDS today and sit down with one of our in-house technologists.
