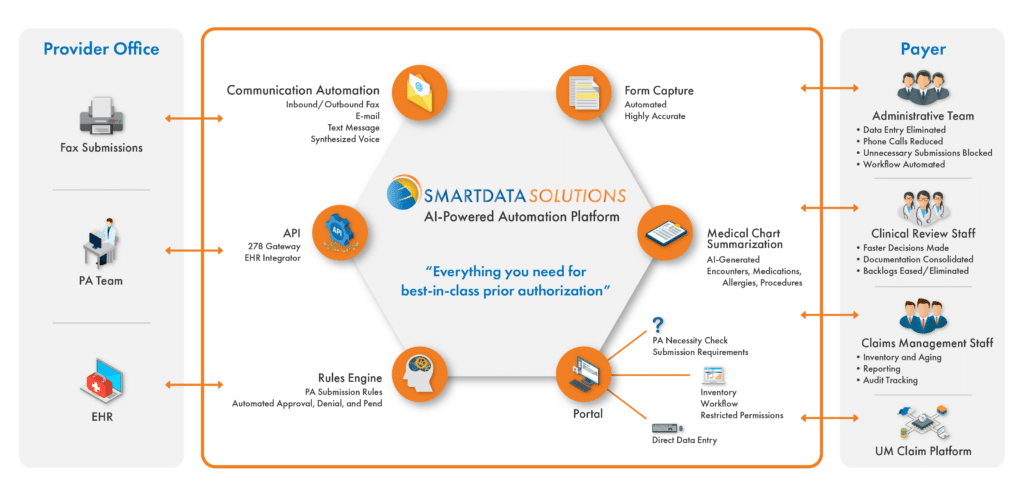
The Smart Data Solutions Prior Authorization Platform solves the most common challenges associated with prior authorization workflows including unnecessary or incomplete submissions, manual data entry, and time-consuming clinical reviews.
With an automated and streamlined decision and communication workflow, you’ll improve your member and provider experience greatly.