Today’s patients expect to receive medical documents quickly after connecting with a healthcare provider or insurance payer. This expectation has grown with the digitization of healthcare throughout the pandemic.
Are your administrative workflows set up to meet the expectations of today’s patients?
Partnering with a claims processing center could be the silver bullet to speeding up workflows for front-end services. Learn how outsourcing front-end services for medical claims processing enhances the patient-provider relationship with fast, reliable communication.
What Are Front-End Services?
The patient-provider interaction starts the moment a patient schedules an appointment. This initiates the processes known as front-end services, including scheduling, patient registration, eligibility, authorization, and checkout.
Front-end staff play an important role as the first impression of the business. Gathering accurate information at each step of the revenue cycle is essential for error-free processing and reducing claim denials down the line.
Factors such as complying with new mandates, the rising cost of management, and transitioning to electronic data interchange have created a boom in outsourcing medical claims management over the last three years, according to Healthcare Finance.
Claims processing centers, specifically medical claims clearinghouses, can serve as the support system between healthcare providers and insurance payers to alleviate common pain points of in-house processing.
Benefits of Outsourcing Front-End Services for Medical Claims Processing
Medical claims clearinghouses speed up workflows, reduce administrative time for in-house teams, and lower the total operating cost for medical claims processing. They can lift and shift administrative workflows to allow in-house staff to focus their attention elsewhere.
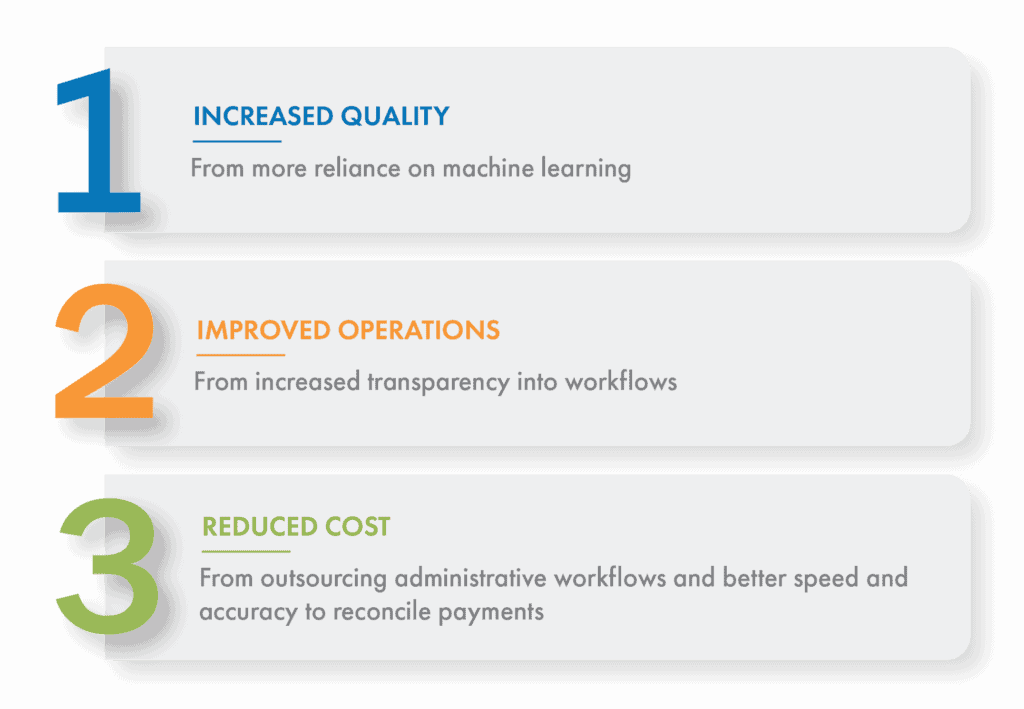
The main benefits of outsourcing front-end services for medical claims processing centers around the speed of business:
- Increased quality comes from more reliance on machine learning to ensure accuracy.
- Improved operations come from increased transparency into workflows, often allowing technology to resolve issues without slowing down processing time.
- Reduced cost comes from outsourcing administrative workflows and having better speed and accuracy to reconcile payments without any hiccups.
Using a medical claims clearinghouse to switch manual processes to electronic yields significant savings for healthcare providers. The potential cost savings per transaction is $8.81 when switching partially electronic workflows to fully electronic, according to the 2020 CAQH Index.
Not only can partnering with a vendor aid cost savings, but it can also increase the accuracy of workflows. Medical claims clearinghouses measure the accuracy of their data capture workloads for reporting to clients. However, it’s important to note that the methods used to measure data accuracy vary from vendor to vendor.
This means when vetting potential partners, a discussion point should be the nuances of data accuracy reporting, such as document level or field level accuracy, only critical fields or all fields, and averages over days, weeks, or months. All of these variables have a great effect on the end metric for data accuracy.
Knowing a vendor’s data accuracy statistics brings peace of mind to teams who share values such as high-quality standards and consistent achievement of front-end service levels.
At Smart Data Solutions (SDS), our robust optical character recognition engines and inline quality control processes are built around service level agreements (SLA), which gives us the ability to monitor these in a way that best works for each business.
Create a Better Patient Experience with 24-Hour Turnaround Times
Every healthcare organization today needs a digital front door strategy to create a patient experience that encourages repeat customers. Partnering with a medical claims clearinghouse for front-end services is an effective way to enhance your healthcare organization’s digital experience.
Medical claims clearinghouses such as SDS can turn around front-end workflows within 24 hours from mail pickup to completion. If a claim needs to go through an appeal, it’s resolved quickly because of our streamlined workflows and support from machine learning. SDS provides expert guidance for optimizing medical claims workflows gained from 20+ years of specializing in claims processing.
When researching clearinghouses, it’s essential to understand the turnaround time allotted for any workflow you’d like to offload. Some vendors only offer 48-hour turnaround or upcharge for faster processing times. At SDS, our standard SLA outlines our commitment to a 24-hour turnaround for front-end services. No matter the vendor, you’ll be able to find turnaround time clearly outlined in any SLA.
Learn more about the AI that powers our 24-hour turnaround time in this interview with OCR Specialist at SDS, Johnny Bouthilet.
