Different types of healthcare correspondence need to be routed to appropriate departments or individuals—and some categories, such as appeals, need to be processed with a higher priority than others.
Processing medical claim appeals is unlike other correspondence processes. Appeals require a specific turnaround time that’s detailed within each jurisdiction. When insurance payers receive an appeal, the clock starts ticking immediately on turnaround time, whether you realize it’s a time-sensitive requirement or not.
Situations like these are one of the benefits of partnering with an experienced vendor to increase workflow efficiency. Partners such as Smart Data Solutions (SDS) have in-house automation and machine learning that exponentially speed up turnaround time and decrease the level of effort needed for processing appeals.
At SDS, our tried-and-true steps for appeals processing simplifies workflows and lifts the administrative burden off of in-house teams. See how partnering with SDS can speed up appeals turnaround time without sacrificing quality.
Defining an Appeals Pre-Process Simplifies the Examiner’s Job
The pre-process is what we call “intake and research” and it involves validating the integrity and quality of the received appeal so that the appeal examiner isn’t wasting time on trivial document review.
Intake and Research Involves:
- Validating that it is an appeal versus basic correspondence
- Validating that the name on the fax cover sheet is truly the insured person being referenced
- If the appeal is for multiple claims, validating that the supporting document is associated with each claim referenced
- Identifying the necessary insured and provider information while also identifying if the appeal is urgent
- Identifying if the appeal is a pre-authorization Rx appeal that may require escalation
- Identifying if it is submitted as the correct level of appeal and not a provider trying to get an immediate resolution
- Sending the outbound letters to providers for the submitted appeals that have issues with some of the data mentioned above
Once the above have their quality checks applied, and access to the various systems needed to validate the data, the pre-process is complete and the appeals examiner can more efficiently process appeals.
Furthermore, the appeals BPO and related technologies at SDS allow us to move quickly through essential steps:
- Validate timely filing
- Check maximum benefit information
- Check/handle U&C issues
- ID appeal types and route to specific workflow queues
- Assist in routing to specialty networks
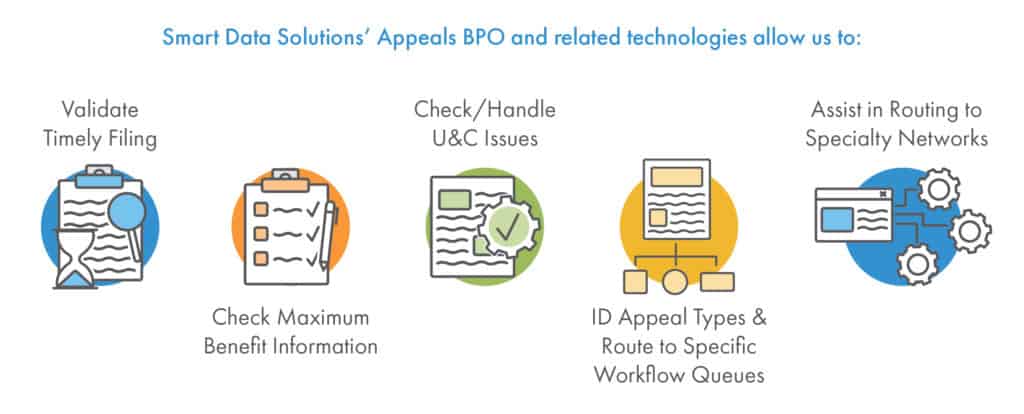
Most of these use our “holding tank” technologies to hold appeals while awaiting further collateral. These steps are essential for correctly processing appeals. When processed manually in-house they can be tedious. However, when outsourced to a vendor, they are simplified and completed efficiently because of automation.
Automation Technologies Speed Up Appeals Processing
Medical claims processing vendors have internal teams that are dedicated to advancing automation technology for more efficient claims processing. While medical documents become increasingly complex to categorize, machine learning can quickly identify documents and process them accordingly. At SDS, we use several automation technologies to increase the efficiency of processing appeals:
- Natural Language Parsing (NLP): NLP assists machine learning with analyzing large amounts of natural language for categorization purposes.
- Optical Character Recognition (OCR): OCR allows machines to analyze images of documents and identify specific typed and handwritten characters. SDS developed a proprietary OCR tool to deliver the highest accuracy possible.
- Machine Learning: Continued innovation in healthcare machine learning assists with determining specific criteria such as member versus provider appeals, and capturing data such as jurisdiction, level of appeal, claim, member, and provider information.
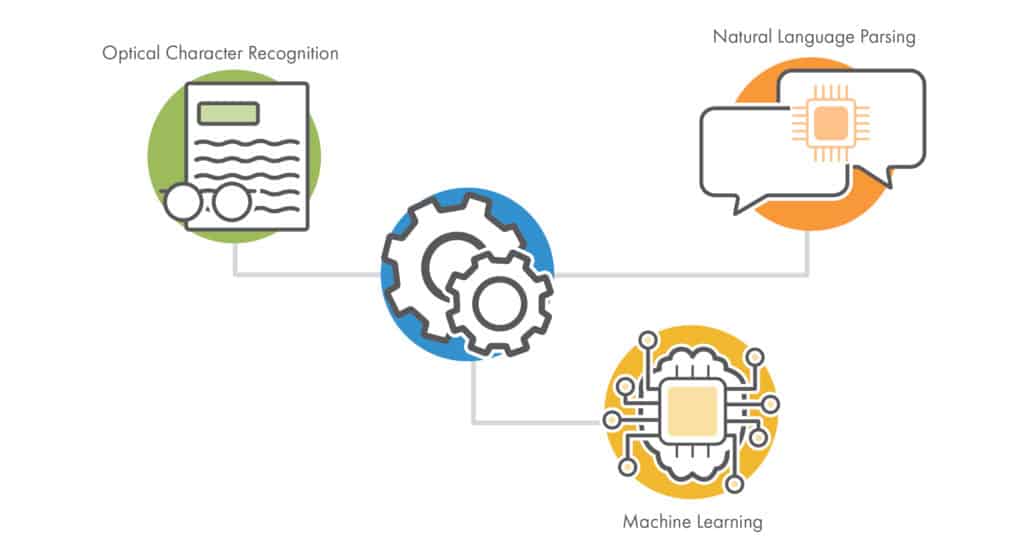
Machine learning enables a more modern, automated process for appeal workflows. In addition to decreasing turnaround time, appeals processing vendors can automate communications efforts such as outbound acknowledgments for a better partner experience. Specific details like these are outlined in service level agreements (SLA) to create shared expectations that meet any business requirements.
Our Proven Process to Decrease Turnaround Time
Embracing automation in medical appeal processing is a surefire way to improve turnaround time, accuracy, and costs. The in-house automation experts at SDS decreased one client’s turnaround time for processing medical claim queries by 72% by bringing structure and automation to the workflow.
With more than 20 years of assisting healthcare and insurance companies with improving medical claims processing, Smart Data Solutions has created a tried-and-true approach to automate appeals intake.
- Analyze and sort documents. First, we run all correspondence through our machine learning document sorting process in order to separate the appeals from the other correspondence.
- Run documents through OCR. Next, we use our multiple OCR engines to capture the jurisdiction, claim, and member data.
- Perform quality control. We supplement our automation process with human-based quality control to achieve 99.5% accuracy and virtually eliminate downstream processing errors.
- Apply business rules. We then apply your business rules to determine the level of appeal, ensure it is not a duplicate, and match it to the member, claim, and provider.
- Send data to the workflow. Lastly, we send the captured data to an existing workflow or host the appeal in our workflow tools.
![]()
Depending on the service level agreement, we can also automate the process of issuing acknowledgments within jurisdictional timeline requirements. The rigorous process Smart Data Solutions follows helps our clients process high-priority appeals quickly, accurately, and with less manual effort.
If your current workflow for appeals processing has bottlenecks or tedious manual steps, our proven approach to appeals processing can help. Contact Smart Data Solutions to discuss how automation can alleviate common pain points of appeals processing.
